By Margaret Dushko, Harvard Law School ‘21
Medicaid 1915(c) Home and Community Based Services Waivers keep vulnerable patients from needing institutional care by providing services at home and in the community like coverage for home health aides and home-delivered meals. Emergency Appendix K modifications present a critical opportunity for states utilizing the Medicaid 1915(c) Home and Community Based Services Waivers to ensure vulnerable patients continue to receive the care they need during the COVID-19 pandemic. These modifications allow states to ensure continued care and to add services and coverage that will help patients stay healthy and safe during this pandemic. We therefore encourage states to take advantage of this opportunity to protect their residents.
Background: HCBS Waivers and Emergency Appendix K Changes
Home and Community Based Services (HCBS) waivers allow states to provide additional services at home and in community settings for Medicaid beneficiaries who would otherwise require institutional care. States can have multiple 1915(c) waivers addressing the needs of different target populations – for example, a state might have one 1915(c) waiver for patients with traumatic brain injuries and another for elderly patients. These waivers can provide a wide range of services, including home health aides, assistive technology, and home-delivered meals.
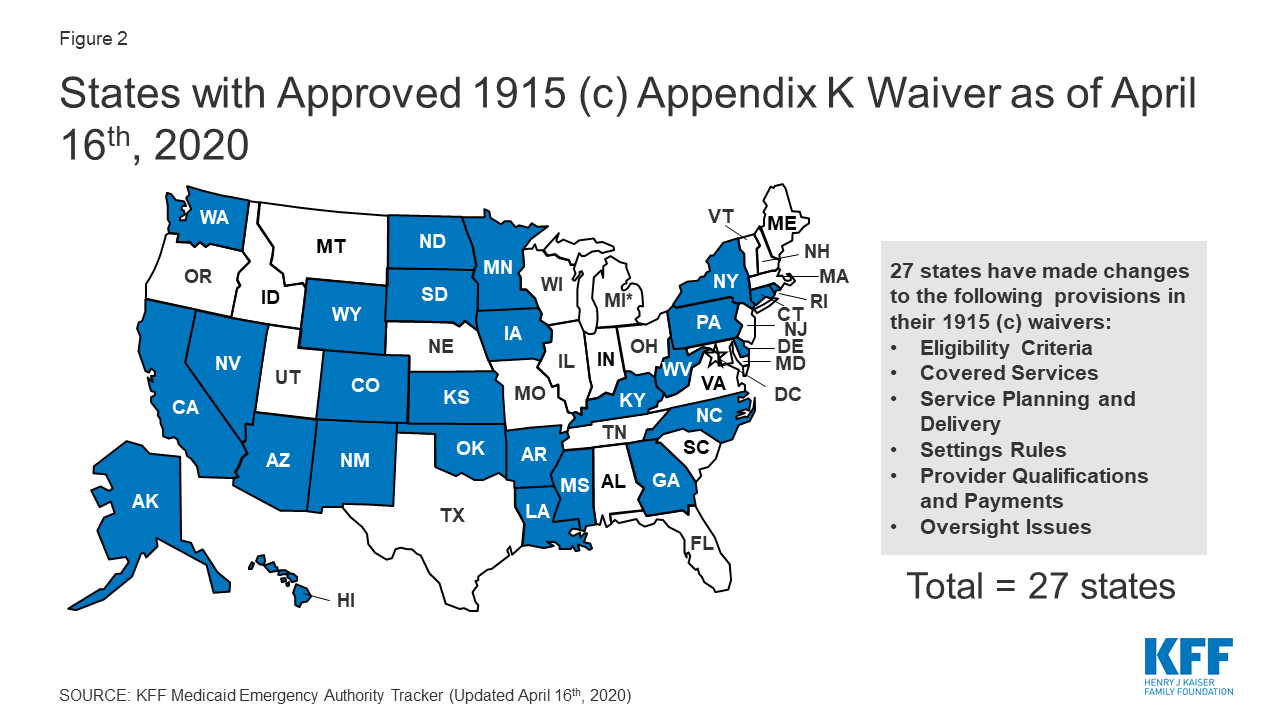
CMS allows states to modify their HCBS waivers in response to public health emergencies like COVID-19 through Appendix K waiver modifications. In anticipation of many states requesting such waivers given the widespread impact of COVID-19 on health care systems, CMS has published a template for COVID-19-related Appendix K changes. This template provides a number of potential changes states can make to their HCBS programs in response to the pandemic.
Because individuals receiving care in institutions have a limited ability to practice social distancing, and providers at such institutions face the same protective equipment shortages facing other health care providers, both residents and workers in long-term care institutions face a higher risk of COVID-19 transmission. Patients in these facilities are often elderly or have serious chronic illness – meaning they are also at increased risk of severe disease resulting from COVID-19 infection. Ensuring that patients at risk of needing institutional care can stay in their homes will help minimize these risks.
Opportunity: Add Home-Delivered Meals
Nutrition is an essential element of health, especially for the most vulnerable patients and particularly now during the COVID-19 pandemic. For example, in a study among hospitalized patients with the same diagnoses, malnourished patients were almost twice as likely to be readmitted to the hospital within two weeks and faced higher mortality rates across the three years following hospitalization. Poor nutrition can also impact the body’s response to infectious disease; studies of previous outbreaks of coronavirus diseases illustrated that diet-related diseases like type II diabetes were associated with more severe illness and higher mortality rates.
With skyrocketing unemployment due to the COVID-19 pandemic, more and more Americans are facing food insecurity, and food banks are struggling to meet the increased demand. Given the importance of nutrition to health outcomes and immunity, it is essential to ensure that everyone has access to sufficient and nutritious food – particularly those patients most at risk of severe disease with COVID-19.
One critical change states can make to their HCBS programs through Appendix K is to add home-delivered meals to the list of covered services. Home delivered meals will directly benefit patients by ensuring they are properly nourished, improving immunity and minimizing the impact of increasing food insecurity on their health. Furthermore, home-delivered meals will allow these patients to more effectively practice social distancing by reducing their need to make trips outside the home for food.
Although CMS has included the addition of home-delivered meals as an option within their Appendix K template for COVID-19, only 8 states have opted to expand meals access in response to the COVID-19 crisis as of April 22, 2020 (Arizona, Connecticut, Delaware, Iowa, Kansas, Louisiana, Mississippi, and Oklahoma). In addition, 4 of the states that have expanded meal access have not expanded access for all waiver participants.
Opportunity: Maximize Eligibility
States can also modify eligibility requirements through Appendix K. Patients should not have to worry about losing their coverage in the middle of a pandemic. Fortunately, almost all states (25/27) that have submitted a COVID-19-related Appendix K amendment to their waiver have allowed remote assessments to take the place of regular in-person assessments. Furthermore, 22 states have extended the timeline for reassessment of patient eligibility to ensure that patients do not lose coverage during the crisis. These changes will help ensure patients already receiving these services maintain their coverage.
In addition to ensuring patients remain eligible for Medicaid coverage of essential services, states should also take steps to ensure that patients can actually receive these services amid the pandemic. Twenty-three states have expanded the types of settings in which waiver services can be provided, and a number of states have made other changes to ensure continuity of care like changing the qualifications needed for service providers or increasing the reimbursement rates for service providers. We encourage all states to take advantage of these modifications to ensure that patients remain covered for such services and receive the care that they need.
States Should Act Now
During a time of crisis, it is essential to protect the most vulnerable members in our community. We urge states – both those who have not submitted Appendix K modifications for their HCBS waivers and those who have not taken advantage of critical Appendix K opportunities – to ensure that their vulnerable residents continue to have access to the care that they need. State Medicaid officers should refer to CMS’s Appendix K page for more information on filing an application and to view approved waivers from other states.